The Increasing Role of AI in Medical Research for Deadly Diseases
The new drugs, surgical procedures and diagnostic processes are vastly superior to those they are replacing.
Summary:
Medical science is changing at a phenomenal rate. The new drugs, surgical procedures and diagnostic processes are vastly superior to those they are replacing. AI is a primary driver in this healthcare revolution.
Many legacy healthcare providers are being left behind. The advancements are coming on so quickly that they are unable to keep up.
If you have a life-threatening disease, you need to be aware of the new therapies, most of which are available in a very few hospitals and research centers.
Emerging Cures finds and get clients access to these new therapies.
Healthcare Institutions Resist Change That Makes Their Services and Skills Obsolete
When dealing with a life-threatening disease, it is the leading edge of medical knowledge applicable to your condition that really matters. AI is the primary driver of exciting, effective new treatments. Research that took months as recently as a year ago now takes hours or even minutes to complete.
Most, but not all, healthcare institutions resist change. They are reluctant to admit that much of their knowledge is obsolete. If they don't know the latest science, they tend to be biased against it. The standard of care is increasingly out of date and irrelevant.
In a recent test on Healthbench, a new, rigorous benchmark developed by OpenAI specifically to evaluate large language models in healthcare scenarios, a simple AI platform designed by Emad Mostaque's company, Intelligent Internet Inc., II-Medical, scored 48%, while physicians, on average, scored 15%. (For more, watch the podcast Moonshots here.)
According to the medical databases Medscape and PubMed Central, total human medical knowledge is now doubling more than once a year:
• 1950: Doubled every 50 years.
• 1980: Doubled every 7 years.
• 2010: Doubled every 3.5 years.
• 2020: Doubled every 73 days.
Groundbreaking research is published daily in hundreds of journals. Advances are being made around the world, around the clock. Clinical trial results are published in a wide variety of databases. Even the most dedicated physicians can't keep up with the deluge of information.
AI Is The Main Driver Of Change In Medicine
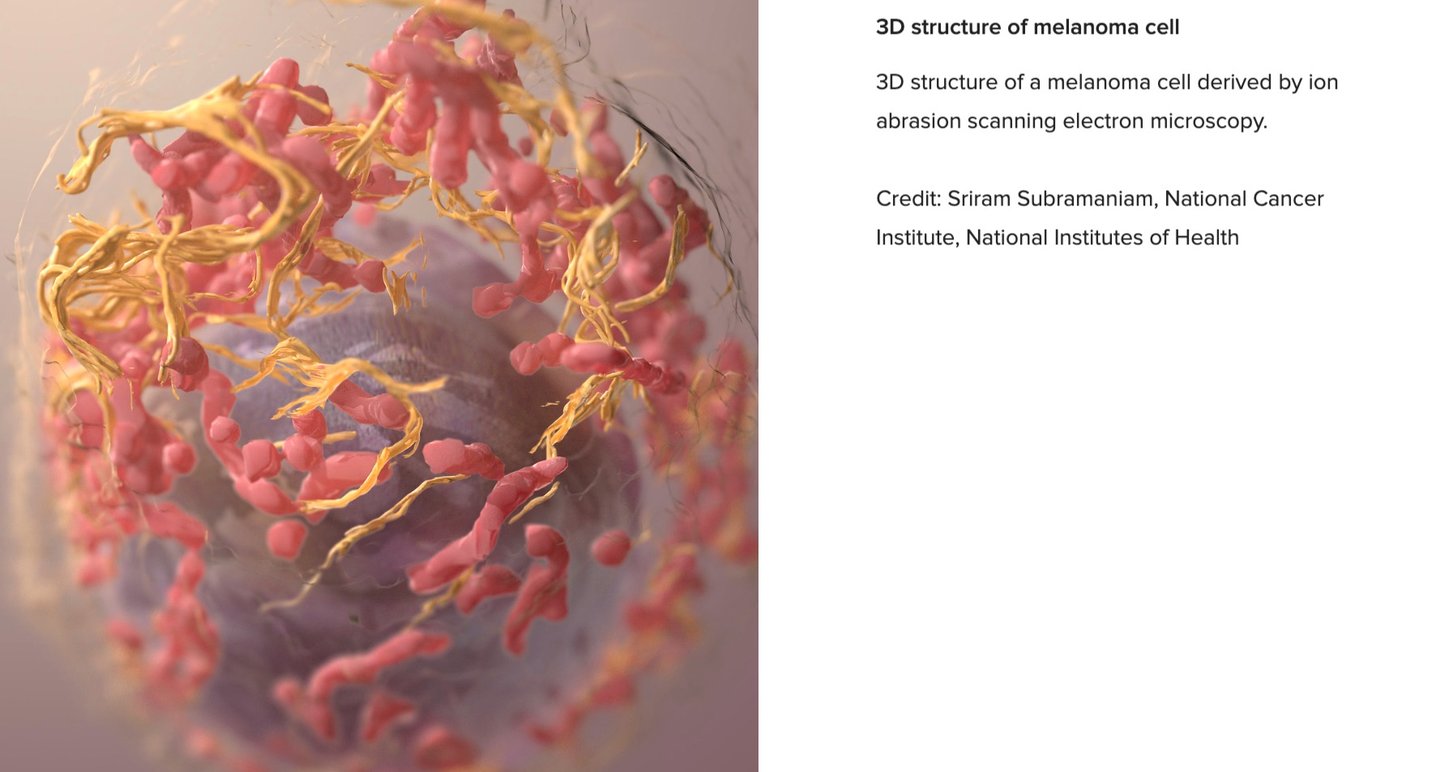
As an example of just one new tool that is having a profound effect: DeepMind's AlphaFold has created 3D images of essentially every known protein in biology (around 200 million), including all proteins in the human genome. Proteins are major factors in both cancer and Alzheimer's. In just a short while, this database has become a critical resource for medical researchers, helping them understand disease mechanisms and develop new drugs and vaccines.
Some other examples of the role AI is increasingly playing in medicine:
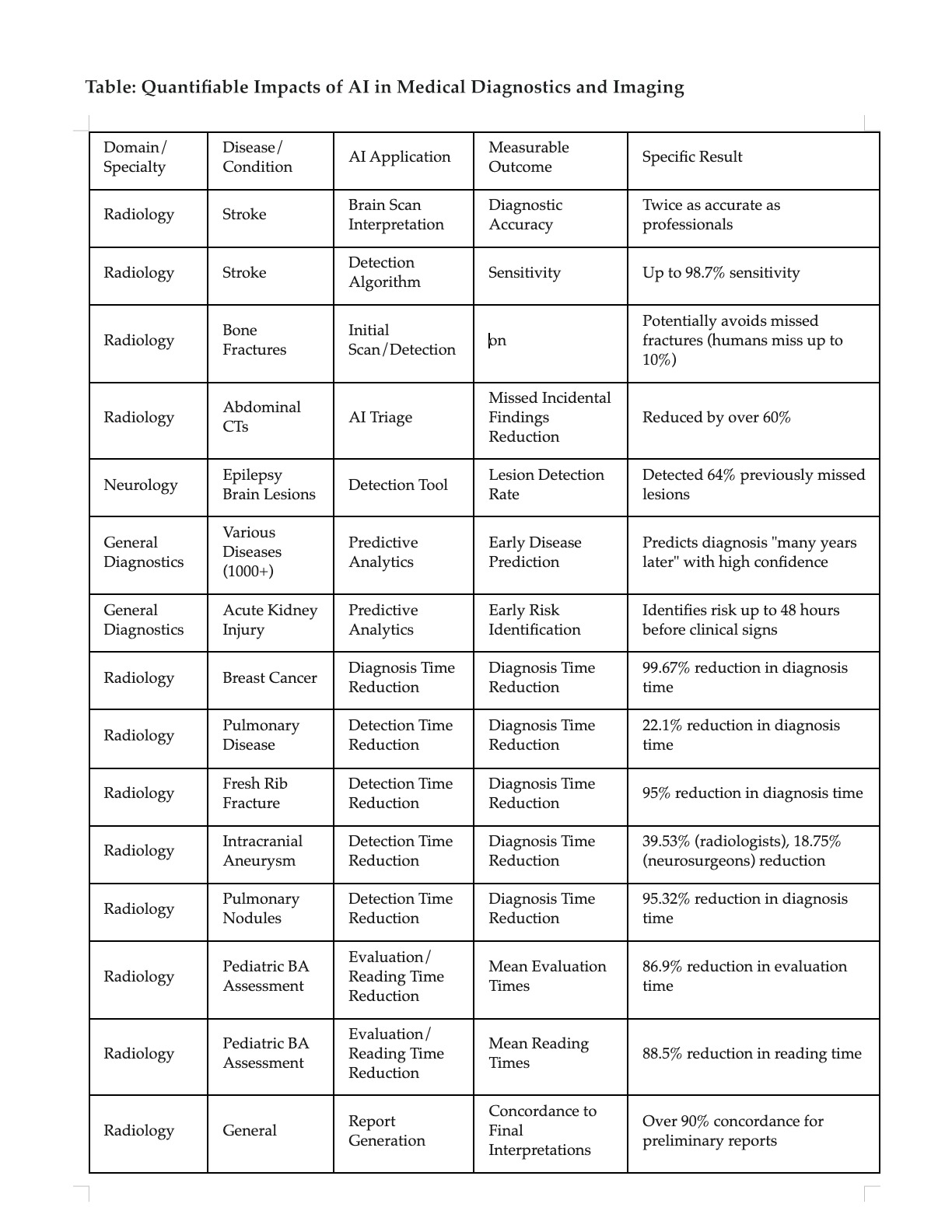
• AI systems are now capable of surpassing human diagnostic accuracy. FDA-cleared systems now reach a 98.7% sensitivity for stroke detection. AI software trained on large datasets of brain scans has proven "twice as accurate" as human professionals in interpreting CT scans, MRIs, and X-rays, and can identify exactly when a stroke occurred, which is necessary in determining medical and surgical treatments.
• Surgical interventions have seen AI-assisted robotic procedures reduce operative times by 25% and intra-operative complications by 30%, while improving surgical precision by 40%.
• AI-powered tools are significantly improving the detection of musculoskeletal injuries. They can spot more bone fractures than humans, a crucial capability given that urgent care doctors reportedly miss broken bones in up to 10% of cases. This AI assistance has the potential to avoid both unnecessary X-rays and missed fractures, streamlining care and improving patient safety.
• In pilot programs, AI triage systems reduce missed incidental findings in abdominal CTs by over 60%.
• An AI tool has successfully detected 64% of epilepsy brain lesions that radiologists had previously missed, identifying tiny or obscured lesions more quickly than the human eye could.
• AI can detect diseases years in advance with high confidence for over 1,000 conditions, often before symptoms manifest clinically. It can, for instance, identify the risk of acute kidney injury up to 48 hours before clinical signs appear, allowing for earlier intervention.
• In breast cancer screening, AI detects breast cancer more accurately, quickly, and consistently.
• In the realm of drug development, AI has accelerated timelines by an average of six months per drug, with some clinical trials experiencing up to 70% cost savings and 80% timeline reductions. AI integration, if implemented nationwide, would generate annual healthcare savings of between $200 billion and $360 billion in the United States alone.
AI-powered symptom checkers can now ask patients a series of questions and suggest appropriate next steps for care. By analyzing patient data, including genetic test results, lab reports, vital signs, and lifestyle factors, AI can identify risk factors and predict the onset of diseases (e.g., sepsis) before symptoms appear. The more widespread this system becomes, the more effective it becomes because data is constantly updated as results come back from the accuracy of earlier determinations.
A Primary Characteristic Of The New Therapies Is Drugs Custom-Designed To An Individual Patient’s Disease and Genetic Characteristics
Advanced therapies are now designed to target specific diseases and devise treatments based on precise molecular targets rather than the application of chemotherapy or radiation that might be effective in one person and fail in another, both with the same diagnosis. In achieving this, AI assesses the cancer’s genetic makeup, and that of the individual patient's, maximizing the effectiveness of the drug and minimizing adverse drug reactions. AI integrated with wearable devices can continuously monitor patient health, detect abnormalities, and even adjust dosage automatically (e.g., insulin delivery for diabetes).
One targeted therapy, monoclonal antibodies, represented 22% of FDA approvals in 2023. These are proteins made in a laboratory and designed to stimulate our immune system. They are used in treating cancer, autoimmune diseases, and infections like COVID-19. These "designer antibodies" are highly specific, binding to a single target, which allows for precise immune responses. In another huge advance in this area, AI was used to design new “binders” that can attach, for the first time, to shape-shifting amorphous proteins, including some implicated in cancer and Alzheimer’s.
Previously, it took drug companies months or years to design binders that attach to proteins. A new AI tool designed by a team from the University of Washington can design binders to grab many previously “undruggable” proteins. (AI-Designed Drugs Can Now Target Previously ‘Undruggable’ Proteins in Cancer and Alzheimer’s, A new AI tool opens the door for designer protein drugs that tackle pain, cancer, and brain diseases. Author: Shelly Fan, SingularityHub). This new AI software recognizes disordered proteins and generates binders to understand the target’s overall shape. It then recombines binding pockets in different configurations to make a library of binder templates. Finally, using a new AI technique called diffusion, it generates roughly a thousand pockets that “allow for trillions of combinations” that can grab onto wiggly proteins, study author Kejia Wu said in a press release.
There are many other examples of how AI processes vast amounts of medical research, genomic data, and scientific literature, uncovering patterns and insights that would be impossible for humans to find manually. AI prioritizes promising drug candidates and eliminates less viable ones early on. It can predict how different compounds will interact with biological targets and estimate crucial pharmacological properties like solubility, bioavailability, and toxicity. AI is being applied to uncover new applications of existing drugs to unrelated diseases, leading to new therapeutic uses, more efficient and successful trials, and bringing new therapies to patients faster.
Some Important Developments Come From Europe and Asia
Therapeutic areas such as oncology, hematology/immunotherapy, and neurological disorders consistently feature prominently among new FDA drug approvals. In 2024, the FDA approved 50 novel drugs, defined as those with active ingredients not previously authorized, alongside nine new cellular and gene therapy products, culminating in a total of 59 new medical therapies. In Europe, this number was 114 new medicines, including 46 novel compounds. A portion of the work of Emerging Cures is finding drugs whose efficacy has been proven in China, Europe, Australia and India and that are now undergoing trials in the US, or are otherwise available here.
Some Important Drugs Don’t Make It Through The FDA Due To The High Cost Of Meeting U.S. Requirements
The pharmaceutical industry spends an estimated $2 billion on average to bring a single drug to market. Companies and individuals behind some worthwhile drugs run out of money trying to get approval. I’m very familiar with one—WF-10. It saved my life. The drug saves lives every day in Thailand but is not available in the US because its sponsor, Oxo-Chemie, ran out of money trying to get through the FDA process. Searchlight Pharma, a company in Canada, now owns the North American rights but is doing nothing with them. (As far as I have been able to determine. I’ve reached out to them for confirmation).
We at Emerging Cures are constantly on the lookout, on behalf of our clients, for drugs that are championed by a respected physician or medical researcher, that are backed by strong data, but that didn’t make it all the way through the approval process for funding reasons. Some of these are available under compassionate release or other programs, either in Canada or the US.
What’s Next?
When I asked one of the AI platforms I use—I believe it was Gemini in this case—what impact AI will have on cancer medicine over the next six to twelve months, this is how it responded:
By mid-2026, AI's presence in cancer research will shift from being an innovative tool to an indispensable partner, driving increasingly precise, personalized, and rapid advancements in the fight against cancer:
Broader Adoption of FDA-Approved AI Tools: More AI-powered diagnostic and prognostic tools, particularly in medical imaging and digital pathology, will gain regulatory approvals and transition from research to widespread clinical use. The European Federation for Cancer Images (EUCAIM) project, aiming to establish a pan-European digital infrastructure for cancer images with at least 50 AI tools by 2026, exemplifies this push for integrated AI.
Advanced Multi-Omics and Multi-Modal AI: AI models will become even more sophisticated at integrating and interpreting truly vast and diverse datasets, combining genomics, proteomics, metabolomics, spatial transcriptomics, and high-resolution 3D imaging data. This will provide unprecedented insights into tumor microenvironments and immune responses, leading to the discovery of more effective targeted therapies and immunotherapies, including novel targets for antibody-drug conjugates (ADCs) and cancer vaccines.
Refined Liquid Biopsy and Early Detection: While multi-cancer early detection (MCED) tests are already advancing, the next 6-12 months will likely see further refinements in their sensitivity and specificity, potentially leading to additional regulatory breakthroughs and expanded trials for population-wide screening. AI will play a critical role in distinguishing true cancer signals from background noise and clonal hematopoiesis, improving the reliability of these tests.
Generative AI's Growing Influence in Drug Discovery: Generative AI models will move beyond simply predicting molecule properties to autonomously designing and optimizing entirely novel compounds with specific desired characteristics. This will further shorten drug discovery timelines and reduce R&D costs, with a higher probability of successful drug candidates entering preclinical and early clinical stages. The "turning point" for AI in precision oncology, as predicted for 2025, will be increasingly evident by mid-2026.
AI-Driven Adaptive Clinical Trials as the Norm: AI will be routinely used to design clinical trials that adapt in real-time to emerging safety and efficacy signals, allowing for faster evaluation of new cancer treatments. AI's role in patient stratification, predicting patient outcomes, and automating trial operations will become more central, making trials more efficient, cost-effective, and inclusive. Wearable technology integration for continuous patient monitoring in decentralized trials will become standard practice.
Focus on Explainability and Trust: As AI becomes more embedded, there will be increasing emphasis on developing more interpretable and "explainable AI" (XAI) models. This will allow researchers and clinicians to understand how AI makes its predictions, fostering greater trust, addressing ethical concerns around bias, and facilitating regulatory approval and widespread adoption.
Ethical Frameworks and Regulatory Evolution: Ongoing discussions and initiatives will lead to more robust ethical guidelines and clearer regulatory pathways for AI in cancer research. This will aim to ensure data privacy, address algorithmic bias, and define accountability in AI-driven decision-making, helping to guide the responsible deployment of these powerful tools.
Conclusion
AI is dramatically accelerating drug discovery, enhancing diagnostic accuracy, enabling personalized treatments, and boosting the efficiency of medical research. If you have a life-threatening disease, you need to fully understand what is happening in clinical trials and emerging therapies relevant to your condition. It might save your life.
Emerging Cures, founded and run by a two-time cancer survivor, finds these new therapies and get clients access to them.
Be in touch if you'd like to talk.
(843) 284-6850 (Office)
(843) 802-0183 (Mobile)
rod@emergingcures.org
17 Executive Park Road, Office 4B
Hilton Head Island, SC 29928
(Small office complex between the fire station and
Stellini's Restaurant)
